OSA 101: A Playbook from Symptoms to Solutions
Part 2 - How is Obstructive Sleep Apnea Diagnosed?
In Part 1 (here) of this series, we broke down what obstructive sleep apnea (OSA) is, who is at risk, and why it matters. Now, let’s dive into how we diagnose OSA. With so many patients at risk and so many undiagnosed cases, identifying OSA efficiently and accurately is crucial. So, what tools do we use, and what do the results mean?
How is OSA Diagnosed?
OSA is diagnosed by “sleep testing.” There are two primary modalities for diagnosing sleep apnea:
🔹 Home Sleep Apnea Test (HSAT) – A simplified test used for moderate-to-high suspicion cases, done in the comfort of your own home.
Home testing has gained traction due to its convenience and accessibility. Typically this involves a wrist-watch like device, finger probe, and sometimes additional equipment around the chest or near the nose. It measures:
✅ Oxygen levels (via pulse oximetry)
✅ Respiratory effort
✅ Airflow and snoring
✅ Body position/movement
🚨 Limitations: HSAT does not directly measure brain activity (EEG) and sleep stages, and in some cases measure airflow through surrogates. There are concerns of variability in results and reliability though overall it is an important/effective tool.
🔹 In-Lab Polysomnography (PSG) – A comprehensive overnight study performed in a sleep lab (similar to hotel room environment). The gold standard for OSA diagnosis, PSG provides a full physiological profile, monitoring:
✅ Brain waves (EEG)
✅ Eye movements (EOG)
✅ Muscle activity (EMG)
✅ Breathing effort & airflow
✅ Oxygen saturation
✅ Heart rate & rhythm (ECG)
🏥 Best For:
🔸 Mild or unclear cases
🔸 Patients with additional sleep disorders (e.g., narcolepsy, complex sleep apnea)
🔸 When HSAT results are inconclusive
Because of resource availability, the vast majority of cases will be diagnosed by HSAT.
DIAGNOSING OSA:
The Apnea-Hypopnea Index (AHI) is the primary metric used to define OSA as a diagnosis and its severity. It represents the number of apnea (complete blockage) and hypopnea (partial blockage*) events per hour of sleep.
🔹 Mild OSA: 5-14 events/hr
🔹 Moderate OSA: 15-29 events/hr
🔹 Severe OSA: 30+ events/hr
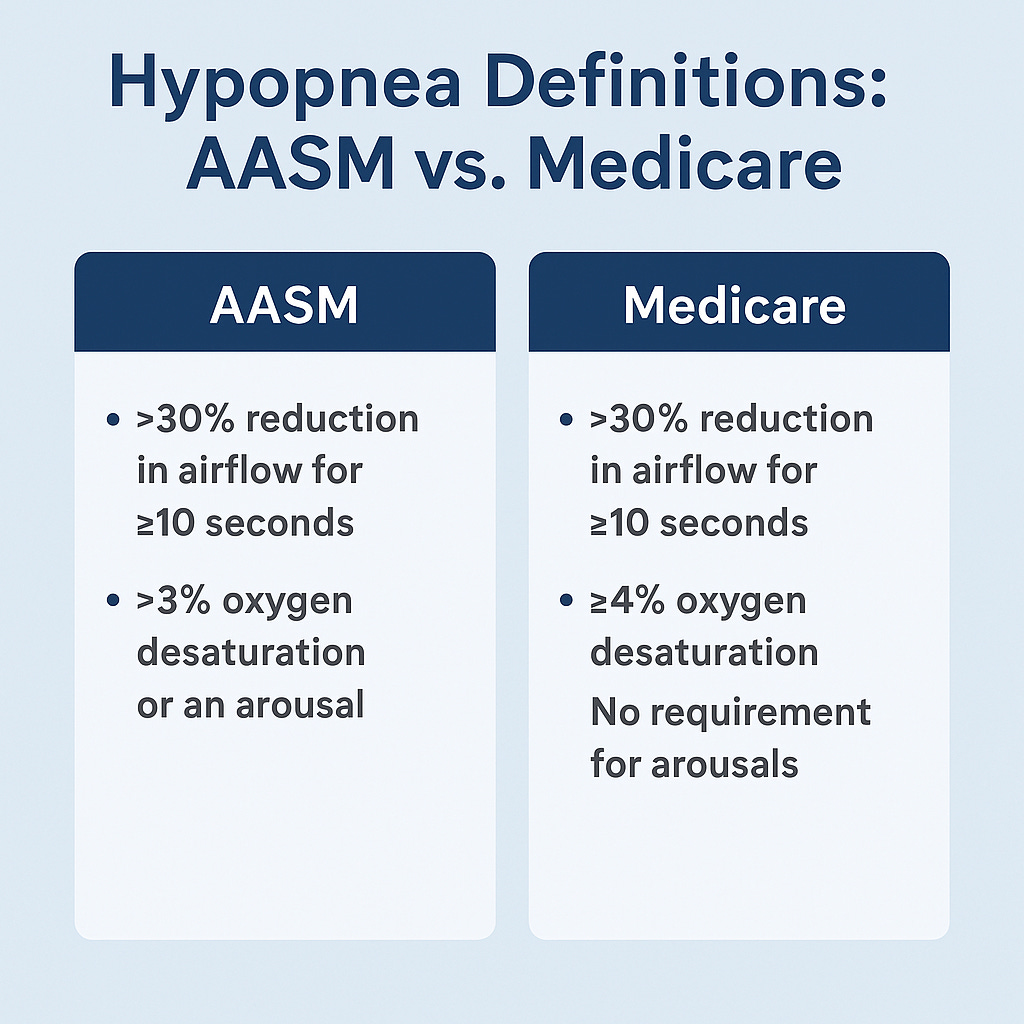
*A Word on Hypopnea: this is going to get a little technical/detailed, but it’s important. The definition of hypopnea has changed multiple times, but currently has two major definitions: the American Academy of Sleep Medicine (AASM) and Medicare:
How Has the AASM Hypopnea Definition Changed Over Time?
Pre-2007: No universal consensus—various labs used different definitions.
2007 AASM Guidelines: Introduced two hypopnea definitions, one requiring 4% desaturation and the other allowing 3% desaturation + arousals.
2012 AASM Update: Strengthened the 3% desaturation + arousal definition (more inclusive).
2023 AASM Update: Still recognizes both hypopnea criteria, but most sleep specialists now use the 3% desaturation + arousal threshold to better capture OSA cases.
Impact of These Differences
The Medicare 4% rule leads to fewer hypopneas counted and lower AHI scores, potentially underdiagnosing OSA in certain patients.
The AASM 3% rule with arousals detects more events, leading to higher AHI scores and likely more sensitive diagnosis, especially in younger and female patients who may have more arousal-based breathing disturbances.
This shift towards more sensitive scoring criteria is majorly important - you can have wildly varying AHI scores on the same sleep studies with the two definitions. It can affect the discussion with patients about the severity of their disease, their risk of health sequelae, and who has insurance coverage for more invasive surgeries. And as of now, there is a lack of compelling studies showing superiority of AASM’s definition in identifying long-term health sequelae.
With the Medicare 4% rule, it is estimated that 25% of males and 9% of females have an AHI>5, while with the more liberal 3%/arousals criteria it was found to be positive in up to 80% middle aged males and 60% of middle aged females!
Is AHI the whole story?
Clearly, not quite. OSA represents a very heterogeneous spectrum - two people with the same AHI may have very different disease burdens. Some key nuances that sleep specialists consider:
🔹 Hypoxic burden: is gaining traction in sleep medicine because it better captures the severity and impact of oxygen desaturations in OSA than traditional indices like AHI. (Greater drops = higher risk of cardiovascular issues). It is calculated using the depth, frequency and duration of oxygen desaturations. Ex. oxygen desaturation index (ODI), percentage of time below 90%, nadir O2 saturation.
🔹 Sleep stage burden: Repeated awakenings fragment sleep, which can limit deep sleep and REM, even if oxygen levels aren’t severely affected. PSG can quantify time/%’s in each stage.
What Happens After a Diagnosis?
Once a patient is diagnosed, we look at the whole picture—symptoms, severity, lifestyle factors—to craft the best treatment plan.
In Part 3, we’ll cover OSA treatment options—from CPAP to new therapies shaking up the field. Stay tuned!
💬 Let us know: What did your sleep study show you? Were you surprised? Drop a comment below!