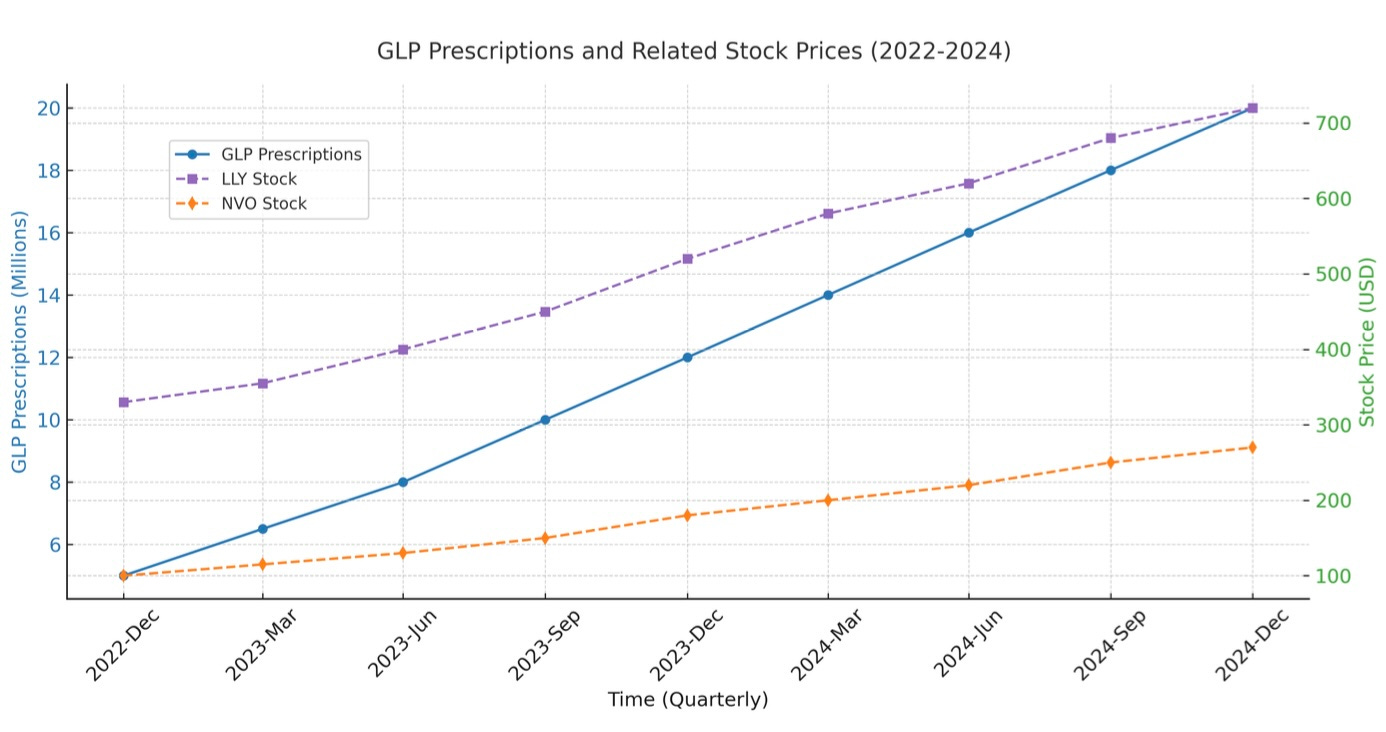
GLP-1 receptor agonists are reshaping modern medicine. Originally designed for type 2 diabetes, their substantial weight-loss effects have propelled them to mainstream attention and explosive uptake. Drug-makers Eli Lilly (LLY) and Novo Nordisk (NOVO) saw their stocks double from 2023 to 2025. Morgan Stanley projects that by 2030, the global GLP market could surpass $100 billion annually. It is estimated that over 15 million Americans are now taking GLP medications.
Weight loss has always been a central tenet of obstructive sleep apnea (OSA) management. While patient age and anatomic factors contribute to severity, increased weight/BMI is strongly associated with worse OSA. Increased fat narrows the upper airway and increases collapsibility, among a myriad of other pathophysiologic effects in these patients. So, the sleep community was excited to hear about the SURMOUNT-OSA study, evaluating GLP drug tirzepatide (Zepbound/Mounjaro) as a treatment for OSA. Published in The New England Journal of Medicine June 2024, the results did not disappoint.
Key Outcomes from SURMOUNT-OSA:
📌 Baseline Stats:
Starting weight: ~250 lbs (BMI 39, severe obesity)
Starting AHI: ~50 (severe OSA)
📌 1-Year Results:
Average weight loss: ~20% (~50 lbs) → BMI ~31
AHI reduction: From 50 (severe OSA) → 20 (moderate OSA)
Hypoxic burden significantly improved (OSA-related cardiovascular risk marker)
Some patients saw their OSA reduced to mild or “cured” *
📌 Takeaway:
This is a HOME RUN study. While not a surprise on the face (losing weight = improved OSA), the degree of improvement and impressive weight loss established GLP’s as a leading treatment option for the large market of overweight OSA patients. The FDA approved tirzepatide for the treatment of OSA in December 2024.
WHAT IT MEANS TO SLEEP PRACTICE
The emergence of GLP’s is certainly affecting sleep specialists and disrupting our treatment paradigm. CPAP (continuous positive airway pressure) is first-line gold standard therapy, with a variety of second line non-surgical and surgical options behind it to help manage OSA**. Weight loss has always been valuable, but the reality is that losing weight is notoriously difficult. Obesity is not simply a failure a will, but a battle against biologic drivers.
Now, enter GLP’s demonstrating significant/sustainable weight loss in patients, overall good tolerance and side effect profile, and with significant public demand. Should these now be seen as first-line therapy for OSA?
I (CG) was asked by a patient last week about this very question. He had severe OSA, had a BMI of 35 (moderate obesity), is not a good surgical candidate, and doesn’t like the idea of CPAP. Doesn’t it make sense to just start a GLP instead of CPAP?
I told him a couple things. First, weight-loss with GLP’s takes time - over a year - so CPAP remains the best immediate treatment for OSA. Second, some patients tolerate CPAP better than expected and can continue it long term. Third, there is no data on the long term use of GLP’s, and the weight loss requires ongoing drug therapy. Lastly, and sadly most importantly, insurers/payers are still deciding who will get coverage for these medications. With that in mind, the reality is many patients don’t want to use CPAP and long-term adherence is around 50%; versus GLP’s that patients are typically eager to pursue as a means to help OSA, as well as improve weight issues that can benefit their lives in other ways.
In my mind, a severe obesity (BMI 40+), severe OSA (AHI > 30) patient is a no-brainer GLP candidate. For the mild/moderate cases of obesity/OSA, it will be a combination of payer coverage decisions (tbd), clinician comfort (growing), and patient demand (HIGH). Regardless, the market for these drugs in the sleep space is likely to be quite large.
MORE TO COME
This is an exciting time for patients, as several new therapies are showing promise. New surgeries will likely be FDA approved this year, and there are emerging oral medications and nasal sprays to improve sleep apnea. As clinicians and scientists, we’re excited to speak on those topics and more. Would you consider a GLP-1 over a CPAP? Comment below - we’d love to hear your thoughts. And continue to follow us, share with friends/colleagues, and tell us what YOU want to learn about.
* We’re hoping this newsletter is of interest to sleep specialists/scientists and the general public interested in improving their sleep. This is a general ‘science/study details are nuanced and important- we’re happy to get into more nitty-gritty in the comments :).
** Opinions our own and not medical advice.