In Part 1 and Part 2 of this series, we explored what obstructive sleep apnea (OSA) is, who’s at risk, and how we diagnose it. Now, we dive into what really matters for patients: what to do about it.
Treating OSA isn’t one-size-fits-all. From minor lifestyle changes to invasive surgical procedures, the “right” choice depends on many aspects, including severity of disease, age, weight, anatomy, and - most importantly - a clear understanding of “why” the patient is seeking care and her/his preferences. This post provides newly diagnosed patients a clear, practical overview of their options.
We often tell patients that ‘cure’ of sleep apnea is exceedingly rare - even with our most invasive surgeries. Our goal is to reduce health burden and enhance quality of life. Treating OSA as a chronic disease allows us to find a successful treatment with patients together.
🛌 First-Line & Non-Surgical Therapies
1. CPAP (Continuous Positive Airway Pressure)
The gold standard first-line therapy for all OSA. CPAP works by delivering pressurized room air through a mask to keep the airway open during sleep (thus preventing snoring/collapse events). It's highly effective in reducing apnea events and improving oxygenation.
✅ Pros: Very effective, widely studied, non-invasive
⚠️ Challenges: Mask discomfort, noise, pressure intolerance. Long-term adherence is around 50%.
Key tip: Mask fit and pressure adjustments can make a huge difference. Ongoing support and coaching improve adherence.
2. Weight Loss & Lifestyle Changes
Weight loss can significantly reduce OSA severity—especially in patients with obesity.
✅ Pros: Broad health benefits beyond OSA
⚠️ Challenges: Requires sustained effort; not always sufficient alone
Bonus: This discussion has changed significantly with the growing popularity of GLP’s (ex. semaglutide/Ozempic) and data supporting their use. I summarize the incredible success of these drugs and them being the “biggest breakthrough in OSA since CPAP” in a separate post here.
Even modest weight loss can reduce the number of apnea events and improve sleep quality significantly.
Reducing alcohol consumption and use of sedatives such as benzodiazepines, is key to improve OSA severity, particularly important in patients who cannot tolerate CPAP.
3. Oral Appliance Therapy (Mandibular Advancement Devices)
These custom-fitted mouthpieces reposition the jaw forward, helping to keep the airway open.
✅ Pros: Comfortable for many, easily portable
⚠️ Challenges: Can cause jaw discomfort or dental changes, especially with prolonged use.
Best for: Mild to moderate OSA patients. Can also be combined with other modalities.
4. Positional Therapy
Some patients experience OSA primarily when sleeping on their back (positional OSA). Solutions range from wearable devices to specialized pillows or even vibrating positional trainers. Ex. MedCline pillow (below)
✅ Pros: Non-invasive, can be effective in mild/moderate positional OSA
⚠️ Challenges: May not work for all; can be uncomfortable; requires consistency
🔧 Surgical Options for OSA
When non-surgical options fail or aren’t viable long term surgery can be very helpful. Patient selection and review of risks & benefits is essential when considering various surgical options. We will do more in-depth discussions of each procedure in the future:
1. UPPP (Uvulopalatopharyngoplasty)
One of the oldest OSA surgeries. It involves removing the tonsils, and repositioning pharyngeal tissues, to widen the airway.
✅ Pros: Reduces snoring and sleep apnea. The surgical procedure with the largest amount of evidence (mostly observational data), demonstrating improvement in clinically relevant outcomes beyond AHI, in particular cardiovascular health.
⚠️ Challenges: Variable sleep test success rates on AHI; significant pain in recovery; possible but rare side effects like swallowing issues
Best for: Patients with enlarged tonsils and non-obese.
2. Hypoglossal Nerve Stimulation (Inspire)
An FDA-approved implantable device that stimulates the tongue nerve during sleep to keep the airway open.
✅ Pros: OSA improvement and satisfaction in appropriate patients, easy post-operative recovery.
⚠️ Challenges: Specific requirements/criteria to qualify. Device requires programming after implant, generator replacement needed approximately every 10 years, not fully MRI compatible, requires continued follow-up. Surgical complications can occur.
Best for: Moderate to severe OSA, CPAP-intolerant non-obese patients.
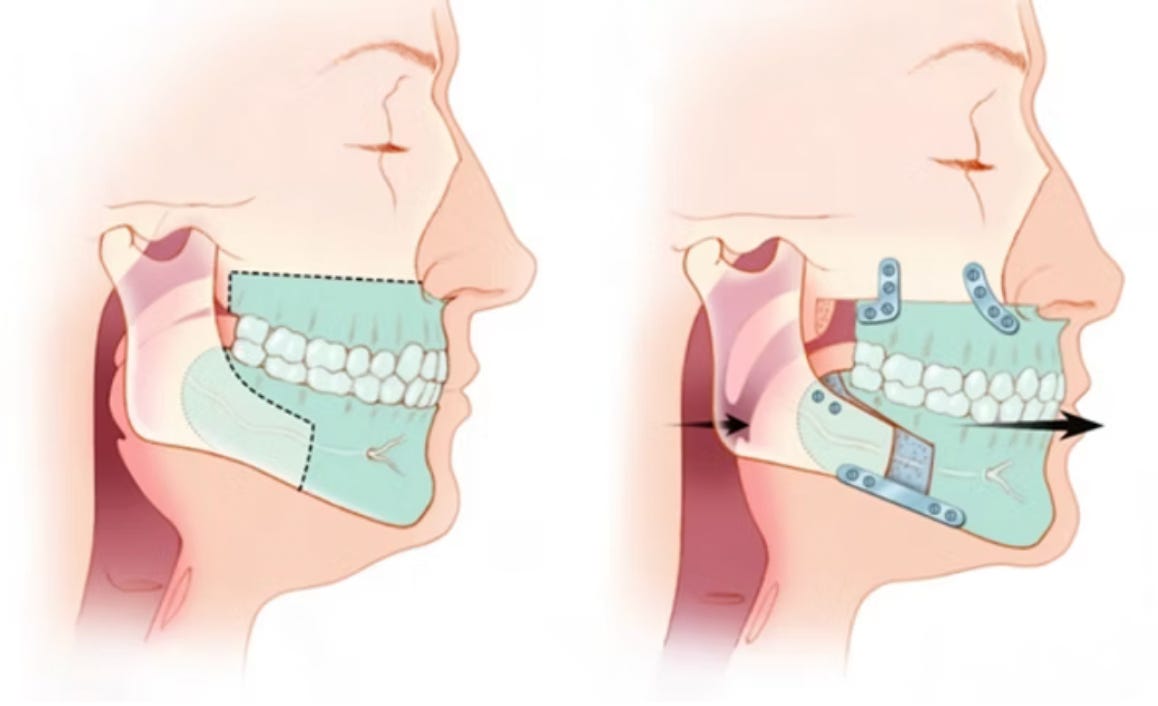
3. MMA (Maxillomandibular Advancement Surgery)
This involves surgically moving the upper and lower jaws forward to enlarge the entire airway.
✅ Pros: One of the most effective surgical treatments; high success in severe OSA
⚠️ Challenges: Major surgery; longer recovery period; facial aesthetic changes, possibility of persistent side-effects such as facial/lip paresthesias.
Best for: Severe OSA or patients with certain facial/anatomical features (e.g., retrognathia).
🎯 Choosing the Right Treatment
There is no “one best” treatment for everyone. A personalized approach with shared-decision making between patient and sleep specialist will lead to the best outcomes.
✨ Final Thoughts
OSA is treatable—and in many cases, very effectively. The most important step is having a clear '‘why’ you need treatment as OSA is a clinical condition, not a “knee-jerk” response to a sleep test, staying informed, and working with your care team to find what fits you best. Know someone newly diagnosed with OSA? Share this guide and follow us for more sleep health information.
Until next time—sleep well.